Infant, Toddler & Child Frenectomy

Airway-Centric Pediatric Dentistry
Dr. Karen is an Airway-Centric Pediatric Dentist with a vast scope of knowledge in tethered oral tissues as well as sleep disordered breathing and growth modification implementation. She has pursued intense continuing education in CO2 laser surgical corrections, breathing pattern assessment, oromyofunctional training, habit cessation therapy and lactation understanding. You must work with a provider with a vast scope of understanding and knowledge, along with a collaborative team approach to provide the ultimate outcomes for your child.


Dr. Karen has dedicated herself to countless continuing education courses, laser courses and clinical shadowing of the leaders in tethered tissue releases. As always, her commitment to excellence and precision is met with Dr. Karen’s deliberate consideration of all aspects of the procedure, the reasons for its need, the surgical release technique, as well and her management of wound healing.
Dr. Karen practices with a collaborative team approach in her patient care. She provides her parents with names of various, highly trained, skilled and experienced professionals in nursing evaluations, cranio-sacral therapies, speech therapies, feeding therapies and myofunctional therapies to provide the most ideal development of your.
Dr. Karen and her collaborative team look forward to working with your children in providing the most optimal oral health, right from the start, when it matters most!
Key points for Dr. Karen’s airway-centric pediatric dental practice:
-
Tongue to spot
-
Lips sealed
-
Nasal breathing
-
Proper posture
All of these correct behaviors lead to appropriate craniofacial development. It is for the maintenance of these key points to proper growth and development that Dr. Karen provides tethered tissue releases and much more!
Dr. Soroush Zaghi, a highly specialized otolaryngologist and sleep surgeon, to give a lecture on pediatric sleep disordered breathing and maxillofacial development, while paying special attention to tongue-tie
Myths about Tongue Ties
-
"Tongue-ties do not actually exist."
-
"Tongue-ties are a fad diagnosis."
-
"Ties do not affect anything."
-
"Ties will go away in time on their own."
-
"If you can stick your tongue out past your lips there is no tie."
-
"ALL ties should be treated."
-
"The Revision will cure everything instantly."
-
"There are NO tongue-tie experts."
-
"Dentists over diagnose them so they can pay for their fancy lasers."
Additional Resources/References:
-
Ankyloglossia and its Influence on Growth and Development of the Stomatognathic System
-
Effects of tongue position on mandibular muscle activity and heart rate function
-
Technical Report: Diagnosis and Management of Childhood Obstructive Sleep Apnea Syndrome
-
Diagnosis and Management of Childhood Obstructive Sleep Apnea Syndrome
-
ADA Policy Statement on the Role of Dentistry in the Treatment of Sleep Related Breathing Disorders

Image: The craniofacial-respiratory complex. (From Garg et al. [33]
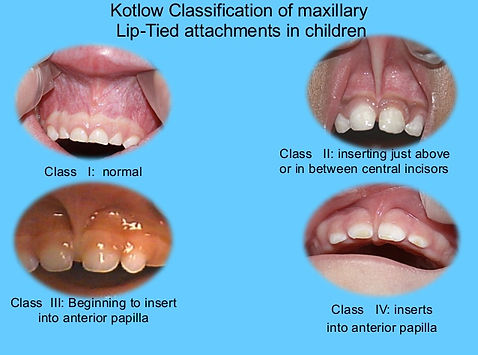


Image: Dr. Saroush Zaghi, MD, The Breathe Institute

Image: Extrinsic Muscles, Netters Anatomy Book

Dosing for Infants and Children









